Diverticular disease is a common digestive condition that sometimes calls for changes to fibre in the diet. Healthy Food Guide nutritionist Kathleen Alleaume shares tips for a healthy low-fibre menu.
What is diverticular disease?
If you’re among the one in three people over the age of 45 who have been diagnosed with diverticular disease, you’ll be familiar with the need to alter your diet when it comes to fibre.
Increasing fibre intake by eating plenty of fruit and veg can help the disease, but if it develops into the inflammatory condition diverticulitis,
a short-term low-fibre diet may be necessary.
Diverticular disease consists of two states together: diverticulosis and diverticulitis.
Diverticulosis occurs when small, bulging pouches called diverticula form in the wall of the colon. Most people don’t have symptoms.
Sometimes it causes mild cramps, abdominal pain or changes in bowel habits, which makes it hard to distinguish from irritable bowel syndrome (IBS).
Diverticulitis is identified through a combination of physical examination, medical history and routine colonoscopy.
When food particles or faecal matter get caught in the pouches and cause them to become inflamed and sometimes infected, the condition develops into diverticulitis, causing sharp pain and digestive symptoms.
Despite having some symptoms in common, diverticular disease isn’t associated with more serious conditions such as bowel cancer.
Diverticulitis and fibre
Two common causes associated with diverticula (pouches) forming are ageing and a low intake of dietary fibre.
“A lack of fibre in the diet can cause constipation, which can put pressure on the weak areas in the colon. An infection may start due to the bacteria in the stool that then get into these diverticula,” says accredited practising dietitian Nicole Dynan, who specialises in gastrointestinal disorders.
While some researchers have linked a high-fibre diet to a reduced risk of diverticulitis, this may not be helpful for someone who is experiencing painful attacks and inflammation.
“During a flare-up of diverticulitis, high-fibre foods can be difficult to digest and can lead to further irritation or inflammation,” Dynan explains. “Restricting high-fibre foods during an episode of diverticulitis can reduce the amount of stool in the colon, allowing the inflamed diverticula to heal. This can help reduce further inflammation or infection.
“The restriction of fibre is a temporary measure. Once the flare-up subsides and the inflammation has resolved, gradually increasing fibre back into the diet is important to help keep the lining of the gut healthy and prevent future episodes of diverticulitis”.
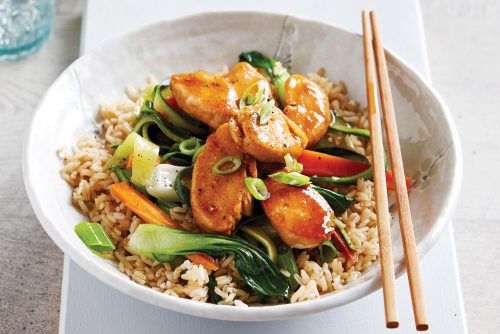
Low-fibre menu
Foods that are typically allowed on a low-fibre diet include cooked fruit and vegetables without skins or seeds, refined grains, lean proteins, dairy products and certain fats and oils. Foods that are typically restricted include whole grains, raw fruits and vegetables, dried fruits and tough meats.
Everyone’s body is different, and what works for one person may not work for another.
It’s important to follow a low-fibre eating plan under the guidance of a healthcare professional to ensure adequate nutrition and avoid any potential nutrient deficiencies.
If you have any concerns or questions about reintroducing fibre into your diet, speak with an accredited practising dietitian.
Can you eat sweetcorn?
Until recently, people with diverticular disease were advised to avoid nuts, seeds, corn and popcorn, due to the risk of them causing a flare-up. More recent studies have shown, however, that these foods are generally safe to eat unless you’re actually having a flare-up.
How to safely reintroduce high-fibre foods
Gradually increase the amount of fibre over several days or weeks as tolerated.
Choose soluble fibre
It is easier to digest than insoluble fibre and less likely to cause discomfort or flare-ups. Examples of soluble-fibre foods include oats, barley, quinoa, beans, lentils and some fruits and vegetables, such as bananas and cooked carrots.
Stay hydrated
Drink plenty of water when increasing fibre in your diet, as fibre needs water to move through the digestive system. The best way to tell if you are drinking enough is to check your urine, which should be pale yellow.
Keep a food diary
Keep track of what you eat and how you feel after eating. This can help you identify foods that may trigger symptoms or cause discomfort.
For more advice on diverticular disease, we recommend: Diverticulitis: Symptoms, causes and what to eat and Digestive problems
Article sources and references
- Better Health Channel. Diverticular Disease. Available at wwww.betterhealth.vic.gov.au Accessed March 2023.https://www.betterhealth.vic.gov.au/
- Dietitians Associations Australia. Diverticular Disease. Available at www.dietitiansaustralia.org.au Accessed March 2023.https://dietitiansaustralia.org.au/health-advice/diverticular-disease
- Diet Vs Disease. Diverticulitis diet. Available at www.dietvsdisease.org Accessed March 2023.https://www.dietvsdisease.org/diverticulitis-diet/
- Gut Foundation. Diverticular Disease. Available at www.gutfoundation.com.au Accessed March 2023.https://gutfoundation.com.au/diverticular-disease/
- Strate L. et. al. 2008. Nut, corn, and popcorn consumption and the incidence of diverticular disease. JAMA. Aug 27;300(8):907-14.https://pubmed.ncbi.nlm.nih.gov/18728264/
- Turner G et.al. 2022. Acute Diverticulitis in Young Patients: A Review of the Changing Epidemiology and Etiology. Dig Dis Sci. Apr;67(4):1156-1162.https://pubmed.ncbi.nlm.nih.gov/33786702/
www.healthyfood.com











