
High blood pressure is a major contributor to heart disease, including strokes, yet most of us don’t even know our reading – or have it regularly checked.
Be honest: have you any idea what your blood pressure is? A month or two ago, I couldn’t have told you mine. Although I’ve written about the importance of ‘knowing your numbers’ for decades, I couldn’t actually remember having my blood pressure taken for about four years.
When I saw a locum GP last month about a minor health problem, he took my blood pressure and started to look concerned. It was 165/100. In other words, very high (see the chart, below). 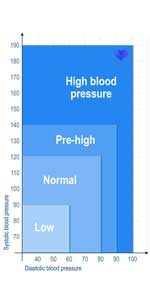
How high is your blood pressure?
Suddenly I was worried, too. I hadn’t been feeling unwell, but my late mother suffered from high blood pressure and in later life had a triple heart by-pass, type 2 diabetes and then vascular dementia. Having witnessed what she went through, I didn’t want to experience the same.
Feeling alarmed, I borrowed a wrist blood pressure monitor from a friend (big mistake, apparently, as this type is notoriously unreliable!). All the readings were consistently sky high, which worried me even more and consequently progressively pushed up my readings, so it was really counter-productive.
Blood tests came next. Luckily, I wasn’t found to have type 2 diabetes or pre-diabetes and had normal liver and kidney function. I did have a cholesterol reading of 6, which is above the normal range of below 5mml cholesterol per litre of blood. An electrocardiogram (ECG) reading was normal, too.
Before putting me on medication, though, my GP booked me in to have a 24-hour ambulatory blood pressure monitor, which recorded my blood pressure every 30 minutes while I went about my daily activities. My blood pressure measured in this way was, in fact, 125/70. It turned out that I’d actually been suffering from a bad case of ‘white coat hypertension’! This is where your blood pressure temporarily spikes when you have a cuff attached to your upper arm due to stress and anxiety about the reading.
Anyway, I was off the hook, but I’m now a ‘work in progress’, changing my diet to keep my blood pressure in the healthy range and lowering my cholesterol and weight. It’s been a wake-up call, but how many people like me are there out there who have no idea what their risk factors are for a heart attack?
The answer is a lot! Experts estimate around 16 million people in the UK – one in four adults – have high blood pressure alone, which is one of the most common risk factors for a heart attack.
What do blood pressure numbers mean?
Bringing down your blood pressure is one of the most important self-help measures you can take to reduce your risk of heart disease.
So, what do the numbers mean? Blood pressure readings have two numbers: the top number is your systolic blood pressure, which is the highest pressure, occurring when your heart beats and pushes the blood around your body.
The bottom one is your diastolic blood pressure, the lowest pressure, when your heart relaxes between beats.
Optimal blood pressure is up to 120/80, but Blood Pressure UK says most people’s reading falls within the range 120/80–140/80. You have high blood pressure if your reading is consistently 140/90 or higher over a couple of weeks.
The bottom line is that even if you have blood pressure in the healthy range, you could still benefit from reducing it in most cases, unless you have low blood pressure (lower than 90/60). In fact, the US Intervention Trial, published in 2015, found lowering systolic blood pressure to 120 rather than the standard target of 140 has reduced the risk of stroke and heart attack by a quarter.
Get your risk factors checked for heart disease
High blood pressure (and also high cholesterol) rarely have any symptoms, so the only reliable way to find out your reading is to have a check-up.
If you’re aged 40 to 74 it’s worth a check-up every five years to assess your risk of heart disease, dementia, diabetes, stroke and kidney disease. This will include a blood pressure check, blood tests for cholesterol levels, blood sugar levels, and kidney function, being weighed (to work out your body mass index) and then being given a percentage risk factor for having a heart attack or stroke in the next 10 years.
If your risk is found to be higher than 10 per cent you will be given diet and lifestyle advice to reduce your risk factors. This will include losing weight, taking 150 minutes of exercise a week, eating a diet low in saturated fat, giving up smoking, moderating your alcohol intake and managing your stress levels. In some cases, though, you will also be prescribed medication (called statins) to lower your cholesterol levels or blood pressure pills.
How to lower your blood pressure
Take the dangers of salt seriously
Salt is the major contributor to high blood pressure because it disrupts the sodium balance in the body. This causes fluid retention, which raises blood pressure.
‘We’re still consuming far too much salt and are regularly exceeding the recommended maximum intake,’ says GP Dr Sarah Jarvis. The health authorities recommend that we don’t exceed 6g salt a day, but most of us eat around 8.1g, a third more than we should, Action on Salt estimates.
‘This worries me greatly as excess salt in the diet raises our blood pressure, and this is one of the biggest causes of heart attacks and strokes,’ says Sarah. ‘High blood pressure frequently has no symptoms, so you may not even know you have it.
‘It’s easy to bury our head in the sand about how much salt we’re consuming. It can seem easier to watch our sugar intake by skipping a dessert than to question the salt content in the savoury food we eat.’
And it isn’t only about savoury items, says HFG nutrition editor Amanda Ursell. ‘We need to be aware that salt is also included in lots of puddings, biscuits and baked goods – which often surprises people,’ she says.
Yet research carried by LoSalt shows that more than half (58 per cent) of us are not concerned about how much salt we’re eating, and 86 per cent of people do not know the maximum that they should be having a day.
‘The public just aren’t aware of how much salt is in everyday foods, so it’s not always easy to know how much salt you’re actually consuming,’ says Sarah. ‘It’s important that we take control of our cooking, the food we eat and how we’re seasoning it to ensure we limit the amount of salt in our diets. By reducing our salt intake to below the recommended maximum, we can make a huge impact on our overall health and blood pressure.’
It’s been estimated that a reduction in salt intake from 10g to 6g a day would be enough to reduce blood pressure, and could prevent approximately 2.6 million stroke and heart attack deaths each year.
6 easy ways to cut back on salt and lower blood pressure
1 Eat fewer processed foods
These are where most of the salt in our diets comes from. ‘Ready meals, ready-made sauces, soups and stock cubes are often high in salt,’ says Sarah. Everyday foods account for 75 per cent of our daily salt intake – rather than the salt we add while cooking.
Take bread, for instance, says Amanda. ‘Look at labels, so you can choose brands with the lowest salt per slice. Around 0.35g–0.4g per 40g slice is about as low as bakers can go from a technical perspective, but a decade ago it could be twice that, so we’ve come a long way.’ Be aware that bread sold loose (often the ‘posh’ brands) with no packaging often has higher levels of salt because, if there’s no need to declare levels, manufacturers can just pile it in. If you’re still getting too much salt from bread, reduce the number of slices you have each day. Also be aware of the salt content in unexpected foods, such as some breakfast cereals, biscuits and cakes.
2 Buy low-salt foods where possible
That means those with no more than 0.3g salt per 100g – those that carry traffic light symbols will have a ‘green’ for salt. Limit foods with 0.3g to 1.5g per 100g (amber traffic light) and, wherever possible, avoid those containing 1.5g salt or higher per 100g (red).
3 Keep processed meats to a minimum. Bacon, ham and sausages, for example, all traditionally contain high levels of salt. The same is true of smoked fish such as smoked salmon and kippers, along with canned
or jarred anchovies.
4 Don’t be duped into thinking gourmet sea and rock salts are better
‘All salt, whether it’s table salt, rock salt, sea salt or pink Himalayan rock salt, is 100% sodium chloride, and it’s the sodium that’s linked to high blood pressure,’ says Sarah.
In many cases you actually end up using more of the rock salt because it tends to come in large flakes, making it harder to control the amount you serve than with fine, standard salt, says Amanda.
‘There are salt alternatives – those, for example, made with potassium chloride and magnesium chloride, such as LoSalt – which can significantly reduce total sodium in the diet,’ she says.
However, one argument against these choices, especially if you like salty food, is that you don’t learn to adjust your palate to enjoying a less salty flavour.
‘Some experts believe cutting back and allowing your taste buds to readjust to lower intakes is a more sustainable approach,’ says Amanda.
6 Check salt levels in cans
Canned veg count towards your 5-a-day, but certain choices may bump up your salt intake. Buy veg canned in water with no added sugar or salt.
If you do use a can of veg with salt, rinse it first (the same goes for tuna). When checking labels, note that sodium and salt aren’t the same: salt is made up of both sodium and chloride.
If labels only state the sodium levels, multiply this figure by 2.5 to get the figure for salt. Or download the free Change4Life Food Scanner app from the App Store or Google Play to check salt in packaged foods.
5 Cook from scratch
Making our own meals helps us control our salt intake. To boost flavour, add spices, herbs or lemon juice to dishes. Cook your own sauces, too, as a lot of salt can lurk in bought varieties.
How the salt stacks up…
6g chicken stock cube = 2.5g
1tsp salt = 5g salt
1tsp marmite = 0.9g salt
1tbspn soy sauce = 2g salt
1tsp bicarbonate of soda = 3g salt
30g portion salted peanuts = 0.4g salt
Other ways to protect your heart
1 Eat foods rich in potassium
Having too little of this mineral in your diet can also contribute to raised blood pressure. Good food sources include fruit and vegetables, potatoes, pulses, yogurt, nuts, seeds and whole grains.
2 Make choices that lower cholesterol
Vitamin E, plant sterols and soluble fibre can help lower cholesterol. Search Portfolio Diet at healthyfood.co.uk to read more about how a combination of nuts, oats, soya and foods such as spreads and yogurts that have added plant stanols and sterols can lower cholesterol by 25 per cent.
3 Lose excess weight
Being overweight or obese raises your blood pressure, putting pressure on your heart and kidneys. Start by switching to wholegrain carbs, being strict about including 5-a-day and sticking with simple fish, poultry and pulse-based dishes and having only occasional lean meat.
Keeping sweets, cakes, biscuits and puddings as treats and avoiding alcohol can usually reduce your calories significantly.
Combine this with more physical activity and weight loss will follow – turn to p76 for our diet plan.
4 Follow a Med-style diet
This is low in saturated fats, salt and sugar with lots of fruit and veg, nuts, wholegrains and seeds, plus lean protein and fish. The DASH (Dietary Approaches to Stop Hypertension) diet takes a similar approach.
5 Get enough exercise
The best types for lowering blood pressure are aerobic activities, including cycling, brisk walking, jogging/running, swimming and tennis.
If you suffer from high blood pressure, avoid exercise that’s intense for a short time, such as weightlifting, sprinting, squash, skydiving or scuba diving.
Health authorities recommend we all aim to do at least 150 minutes of moderate exercise per week.
6 Quit smoking and cut back on booze
Smoking and too much alcohol raise BP
7 Ask about medication
If your blood pressure is consistently very high you may need medication, such as ACE inhibitors and ARBs (angiotensin receptor blockers
Case study
I‘ve been given a second chance❜
When UK footballing legend Glenn Hoddle collapsed on his 61st birthday, the sporting world was stunned.
The ex-England and Tottenham player and manager had kept himself in good shape, swimming three times a week, working out in the gym and playing golf regularly.
He was a vegetarian, a non-smoker and maintained a healthy weight. Frankly, Glenn was the last person you’d expect to have a cardiac arrest. But immediately after recording a football pundit show for BT Sport 12 months ago, his heart stopped, and he fell ‘like a starfish’ back on the floor. He cracked his head as he fell, leaving fellow football pundits Paul Ince and Harry Redknapp, who were with him, utterly horrified.
Luckily for Glenn, there was a sound engineer at the BT Sport studios called Simon Daniels, who is a special constable in his spare time and had done First Aid training.
Simon was able to give cardiopulmonary resuscitation (CPR) immediately to restart Glenn’s heart and then shock it back into normal rhythm with a defibrillator before the paramedics arrived minutes later.
A few of Glenn’s ribs were cracked, but the prompt action saved his life (chances of survival fall by 10% every minute you go unattended following a cardiac arrest).
His football colleagues shouted at Glenn to stay with them and keep going… They were convinced he heard their encouragement as they saw his eyes flicker even though he was unconscious.
No warning signs
‘I’d felt perfectly well that day and in the weeks running up to it,’ Glenn tells HFG.
‘I really had no clues. I didn’t feel hot or cold or dizzy – that’s why it was all such a big shock. I’d had a check-up about a year before and the only issue the tests showed was that I had slightly raised blood sugar. I was told I should keep an eye on it. No problems with cholesterol or blood pressure were detected at all.
‘I’ve been taking medication for the irregular heartbeat condition AF (atrial fibrillation) for about 15 years, but that was under control and I was feeling well.’
Hidden heart disease
Doctors later discovered from an angiogram that Glenn’s heart attack was the result of having blocked arteries caused by coronary heart disease.
‘My consultant told me they didn’t know why I hadn’t had a massive stroke before, as three of my four arteries were completely blocked and the fourth was only functioning at 1%,’ says Glenn, who underwent a quadruple by-pass operation 10 days after the attack.
‘I’d had no idea, and that’s what’s so frightening. I was just going to work as normal, unaware that I was at risk. I’d never been one to eat fry-ups and would only have an Indian takeaway once every few weeks. I didn’t add salt to my food, either, and only drank red wine with meals when eating out. I’d never smoked. I was totally shocked.’
After his operation, Glenn was given diet and lifestyle advice.
‘I thought, here we go – they’re going to tell me to stop eating lots of things. In fact, the advice was more about adding foods to my diet – particularly fruit and vegetables and especially greens like broccoli and spinach.
‘I’ve cut back on saturated fat and have switched to a low-fat spread. I also check the salt content of processed foods.
I was never one to pick up the salt cellar anyway or pile salt on my food as you see some people doing, but I wasn’t aware before just how much salt is added to processed foods and other staples such as bread. That’s what creeps up on people, really. They think about the fat and sugar they’re eating but not so much about salt. At home now we use Lo-Salt and low-fat products.
‘I do have a sweet tooth. I still have a bit of chocolate, but not the amount I used to have when I was a football manager and always on the road, picking up chocolates and crisps from petrol stations.
‘I make sure I maintain my fitness. I do a lot of swimming – probably about three times a week – which I find gets my heart and lungs going, and I go to the gym. I play golf, but at the moment I use a buggy – I can walk 3 or 4 miles on the flat now, but not the 6 to 8 miles around the golf course. I’m hoping to get back to that soon.
Take the time to get checked
‘I’m so lucky still to be here. I feel it wasn’t my time, and I’ve been given this second chance. I’m now almost fully recovered. My only slight concern is I can get breathless on hills or going up stairs, but I’m hoping my medication will improve this. I’m taking tablets for blood pressure, cholesterol and my AF.
I also regularly take my blood pressure readings at home with my own monitor.
I think there has to be more emphasis on prevention and persuading people to get their blood pressure checked and their cholesterol and blood sugar measured.
Men don’t tend to get checked out. They’re more likely to get their car MOT-ed before they have their body looked at, which is ridiculous, really.
And I was one of them. I’ll be honest – I didn’t like going to the doctors. But, my word, after what I’ve been through… If you can prevent that, it’s worth half an hour of your time.
‘For me now it’s really important to highlight why we should all be checking our blood pressure regularly and making sure we know our numbers. It only takes a couple of minutes to take your blood pressure and it can be done at home or at your local pharmacy or, of course, by your GP.’
Glenn is a brand ambassador for Lo-Salt.
Article sources and references
- National Health Service (2019) High Blood Pressure (Hypertension)https://www.nhs.uk/conditions/high-blood-pressure-hypertension/
- Blood Pressure UK (2019) Blood pressure and youhttp://www.bloodpressureuk.org/BloodPressureandyou/Thebasics/Whatishigh
www.healthyfood.com










